Demystifying Breast Cancer Screening Options for Women: Mammography, Ultrasound, and MRI
Or, too many options is confusing!
A physician colleague in my multi-specialty group emailed me:
“I’m due for my mammogram, but every time I have one, a screening ultrasound or MRI is recommended, too. Can I skip the mammogram and just get the MRI?”
[She gave me permission to post her edited email to help other women grappling with this common question.]
If a single test finds cancer best, do it.
But, screening for breast cancer has morphed and now includes extra screening options like screening breast ultrasound and screening breast MRI.
Why three screening tests? Which one is the best? Can I just do the best one?
And the ultimate question:
What do you recommend to your wife or mother?
Let’s delve into this more, understand different scenarios, and reach an actionable conclusion.
Introduction
Breast cancer screening is essential for early breast cancer detection and improved treatment outcomes. Mammography is a common screening test, but has its limitations. Screening breast ultrasound and abbreviated screening breast MRI emerged to increase cancer detection rates. Let’s simplify these screening options and help you make informed decisions about your breast health.
Mammography: The Standard Screening Tool
Mammography is a good screening test for breast cancer, but not perfect. Mammography detects 5-7 breast cancers per 1000 women screened each year. It is still the first recommended option because it is better at detecting Ductal Carcinoma In Situ (DCIS) than MRI. However, mammography alone may not suffice for women with dense breast tissue.
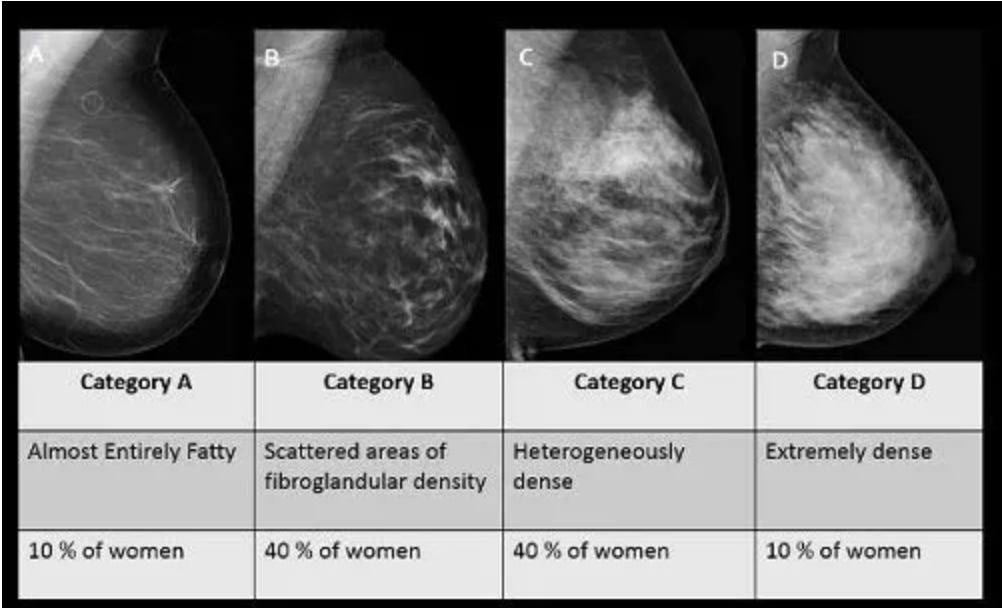
This infographic from the University of Wisconsin explains breast density. Breast cancer most commonly develops as a white mass or white calcifications that look like white specks. Can you find a white mass in the category D or category C breast? I struggle with it. In my radiology practice, computer software reads every woman’s breast density to decide what their density is so we can offer more screening options for women with category C or category D dense breasts. We offer either screening breast ultrasound or abbreviated screening breast MRI.
We do something extra and separate from breast density in my practice — we calculate each patient’s lifetime risk of breast cancer. Every woman who undergoes screening answers Tyrer-Cuzick risk score questions. An example risk assessment is here: https://ibis-risk-calculator.magview.com/ A database provides a woman’s 10-year and lifetime breast cancer risk. Data shows women with a greater than 20% lifetime risk of breast cancer benefit from breast MRIs.
Breast density and lifetime risk are separate risks for breast cancer. When breast density makes it hard to see cancer, that’s one type of risk. Lifetime risk scoring like Tyrer-Cuzick is assessing for a different type of risk — genetic risk.
Knowing this difference, let’s learn more about ultrasound and MRI.
Breast Ultrasound: An Additional Tool
Automated Breast Ultrasound (ABUS) is an option for women with category C and D dense breast tissue. ABUS detects 1-2 additional cancers per 1000 women when used after mammography. While it is not as effective as MRI, it offers an alternative for women who cannot undergo MRI due to metallic implants, claustrophobia, or contrast allergies. Moreover, insurance often covers ABUS, making it a more accessible option for many women.
ABUS relies on ultrasound, or sound waves, to create images of differences in tissue interfaces to help radiologists find cancer that mammography might have missed. It’s not as limited by breast density. The exam takes 10-20 minutes and involves lying face up on a table while a machine or an ultrasound technologist takes pictures of both breasts.
Breast MRI: The Superior Choice
Breast MRI is a powerful screening tool that comes in two flavors: diagnostic and abbreviated (ABMR). Diagnostic MRI is for women with a lifetime breast cancer risk greater than 20% or for cancer staging purposes. ABMR, on the other hand, is designed for women with dense breast tissue. It is a shorter, less comprehensive exam than the diagnostic version.
ABMR detects 5-10 additional cancers per 1000 women after mammography, making it a superior choice to ultrasound. In some trials, it has even found up to 17 additional cancers per 1000 women. Although insurance coverage for ABMR has improved, it may still not be accessible to everyone.
ABMR involves entering an MRI scanner, which is a powerful magnet. An IV is started and we give contrast during the exam. Cancer takes up contrast and is better seen with MRI than mammography or ultrasound. ABMR takes 5-10 minutes and involves lying face down on the MRI table for the test.
The Ideal Screening Paradigm: A Combination Approach
Given the strengths and limitations of each screening method, the ideal approach for most women would be mammography, followed by ABMR. This is what I recommend to my wife. This combination maximizes cancer detection rates while minimizing costs and exposure to imaging. Although unconventional screening paradigms, such as alternating between mammography and MRI every three years, have been proposed, they are still experimental and may not become widely accepted.
Expert strategy: Women who undergo mammography and breast MRI in my practice commonly alternate the exams every six months. In other words, they get their screening mammogram around January 1, then get the breast MRI around July 1. That way, they’re only 6 months from another look for cancer.
Actionable conclusion
Understanding the available breast cancer screening options is crucial for women in making informed decisions about their health. Mammography remains the first choice, but adjunct tools like ultrasound and MRI can improve cancer detection rates.
Mammography and ABMR together offer the best chance of early detection and better treatment outcomes for women with category C or D breast density. Always consult with your healthcare provider to determine the most suitable screening plan based on your unique risk factors and personal preferences.